Meet Valeda: The First FDA Approved Treatment for Vision Improvement in Dry AMD
dry macular degeneration 10:34
An estimated 19.8 million Americans over the age of 40 have a diagnosis of macular degeneration (AMD), which can cause significant central vision loss as the disease progresses from year to year. Genetics, lifestyle, and diet are all major risk contributors, but the older we live, the aging process also plays a significant role in our increased risk of AMD. By age 80, 30% of Americans have macular degeneration. A number of treatments have changed the way we manage macular degeneration and preserve the vision of those affected. Anti-VEGF treatments for wet macular degeneration are the standard of care to preserve and in some cases even improve vision. Dry macular degeneration has been historically without treatment, but in 2023 the FDA approved two treatments for the most severe form of dry AMD, geographic atrophy, which can slow the worsening of this condition but did not show any vision improvement. So for the the majority of patients with AMD (90% of Americans have the dry form of the disease), there has been no treatment that could improve or restore any vision that person had lost.
Until now.
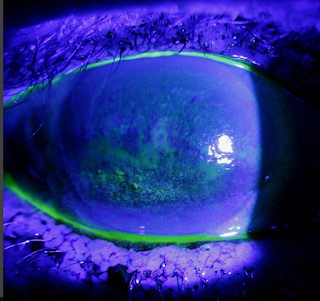
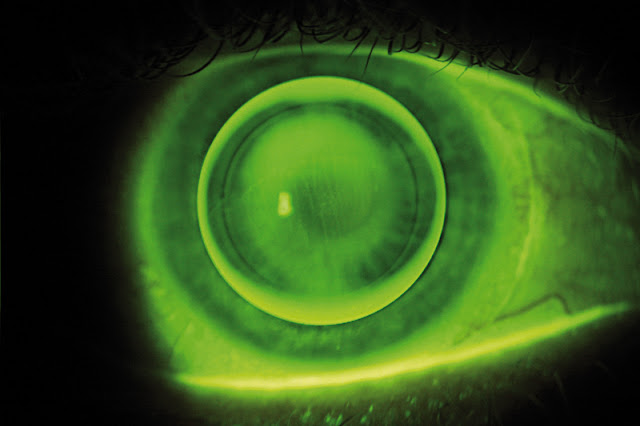
On November 5, 2024, the FDA approved the Valeda Light Delivery System as the first ever treatment for vision improvement in patients with dry AMD. The treatment is for patients in the early stages of dry AMD that have no progressed to geographic atrophy. The device uses photobiomodulation, a treatment currently used in arthritis, wound repair, physiotherapy and sports medicine, which targets the mitochondria at the cellular level to stabilize metabolic cellular function. In AMD, the macular photoreceptor cells are struggling to metabolize light energy and free radical damage, resulting in the build up of waste and debris (drusen) at the macula, inflammation, and is the condition advances, scar tissue (geographic atrophy) and bleeding inside the eye (wet macular degeneration). By targeting the mitochondria of macular photoreceptor cells to increase metabolism, increase ATP (energy!) production, and boost cellular repair in response to light and free radical damage, tissue function is better preserved and protected. Using this photobiomodulation approach, the Phase III LIGHTSITE trial showed that patients gained an average of 5 letters of improvement in vision over a 2 year period using the device. Let's break down the data from this pivotal study:
The LIGHTSITE III trial was a double-masked, sham controlled, multi-center study that was run at 11 eyecare centers across the United States and included 100 patients (148 eyes) with early or intermediate stage dry AMD. Included study participants were age 50 or older (average age was 74.4), and have best corrected vision of 20/100 to 20/32 Snellen Acuity. Patients with geographic atrophy or wet AMD were not included in this study. If a patient had significant cataract that would affect vision or would require surgery in the next 2 years, or a history of other eye conditions or diseases that can affect vision including glaucoma, retinal vascular diseases, macular edema, amblyopia (lazy eye), or nystagmus), they were also excluded. Because the treatment is light-based, any patients that had light sensitivity disorders (including history of seizure, epilepsy, or migraine) or that were taking photosensitizing medications could not participate.
 |
| The Valeda device is an in office treatment that stimulates improvement in cellular metabolism. Currently available in Europe and South America, this device is now FDA approved and will be available in the USA at eye doctor in the near future. via |
Treatment: Subjects were given in office treatments with the Valeda device using photobiomodulation at 3 wavelengths: 590 (yellow), 660 (red), and 850 nanometers (near infra-red), or a Sham treatment that emitted much less light (the sham mode delivered 50x less 590 nm, 100x less 660 nm wavelengths and no 850 nm wavelengths). Participants received these treatments over 9 sessions spaced over 3-5 weeks every 4 months for a period of 24 months.
Results: At 13 months the Valeda-device treatment group had a statistically significant improvement in gained visual acuity over the sham treatment group. At month 13 patients had received 4 series of treatment, and the average change from baseline in best corrected vision was +5.4 letters in the treatment group, versus +3 letters in the sham group. Over half (55.5%) of patients in the treatment group increased vision by more than 5 letters: 26.4% of the treatment group had 10 or more letter gain, and 5.5% had a 15 or more letter gain in best corrected vision. At 24 months, these results were sustained, with an average improvement of 5.9 letters from baseline in the treatment group.
In addition to an improvement in best corrected vision, the treatment group also showed a reduced risk of vision loss over the study period. Only 7% of treated eyes lost more than 5 letters during the 24 months of the study, versus 18% of the sham treatment group who lost more than 5 letters of best corrected visual acuity.
Also, significantly fewer of the Valeda device treatment group went on to develop geographic atrophy over the 24 month study. 6.8% of the treatment group developed geographic atrophy versus 24% of the sham group.
The device was well tolerated with 3 participants having device-related adverse events- all of which were dry eye in nature. 5 of the study participants with treatment went on to develop wet AMD versus only 1 of the sham group, but these results were not deemed to be statistically significant on review (treatment versus sham group enrollment was 2:1).
Stay Tuned: Now that this device is FDA approved, the developer LumiThera will need time to ramp up production and develop access channels. You can sign up on their website to get updates about device availability. They also have a Valeda locator on their website (but right now no offices in the United States are listed).

.png)
.png)




.png)




























.jpg)